Busting 6 common myths of the telemedicine sector
According to data shared by Frost&Sullivan, the number of telehealth visits grew by 50% in the UK alone in the first months of 2020 and the number in the US will grow by 64.3% by the end of the year.
Almost every type of medical clinic now offers the opportunity to contact doctors, including physical therapists and dermatologists, via a video conferencing tool or an online communicator. Other research seems to be supporting the idea that the sector will be growing even more in the next few years – Business Wire predicts that the global telehealth industry will be worth 12 million USD in 2023.
The sector is growing rapidly in the pandemic, but its overall adoption rate in most of the countries has been slow, with only 17% of UK-based doctors using the solutions in 2019 (Frost&Sullivan, 2020). It seems like the biggest usage of telehealth solutions has been observed in places where access to traditional medicine is limited, so it’s been an add-on rather than an alternative to on-site visits.
It’s also clear that telemedicine will never be able to replace traditional medicine, but a growing list of tools such as heart rate and temperature monitoring devices and surgical robots that are now widely used for remote procedures, give us a glimpse into what the future of the health industry may look like. As do the self-assessment tools that can be crucial for early detection of any disease, including Covid-19.
There is still some wariness surrounding this sector, and I’d like to bust some of the common myths in today’s article.
Telemedicine is a new sector
Let’s break the first myth that telemedicine is a new, up-and-coming industry. That’s not true, telemedicine has been used for many years, it’s just that it has not been mainstream.
The fact that telemedicine is not new makes it more reliable. There are existing videoconferencing, online payment, messaging and documentation tools that can be safely and easily adapted to the needs of any healthcare practice, no matter how big or small.
This also means that these solutions have been tested with a large group of patients, including the elderly and children, supporting underserved communities for years i.e. in West African countries.
The fact that telemedicine has been used for years doesn’t mean that it doesn’t employ modern technologies and tools. One of the solutions we’re working on at Spyrosoft is a remote diagnostics process that uses Artificial Intelligence algorithms for clear-cut and precise movement, sound and image tracking.
As I’ve mentioned, more time to develop telehealth solutions means that they’re tried and tested. At Spyrosoft, we’re working in accordance with ISO 13485. Spyrosoft QMS provides both the workflows and standard operating procedures you need to ensure compliance at all phases of the product lifecycle.
Telemedicine is expensive
Even a few years ago we couldn’t confidently assert that using telemedicine solutions are cheaper than traditional methods. However, that’s no longer the case. I’ll admit that telehealth requires investment when introducing the model, purchasing devices and setting up data monitoring systems. However, once these are in place, you can save on the costs of maintaining a medical facility.
The financial factor has been one of the main reasons for the slow adoption rate of telehealth with these solutions being around 10% more expensive than traditional ones. The overall funding necessary to start a telehealth programme has reduced, and I’m sure that we will see a few more companies in the next few months working to decrease them even further.
Telemedicine worsens the patient experience
An important aspect of telemedicine: patient experience can be easily improved by using telehealth solutions. From a technical point of view, this is how the patient circulation data flow looks for any type of medical device developed at Spyrosoft:
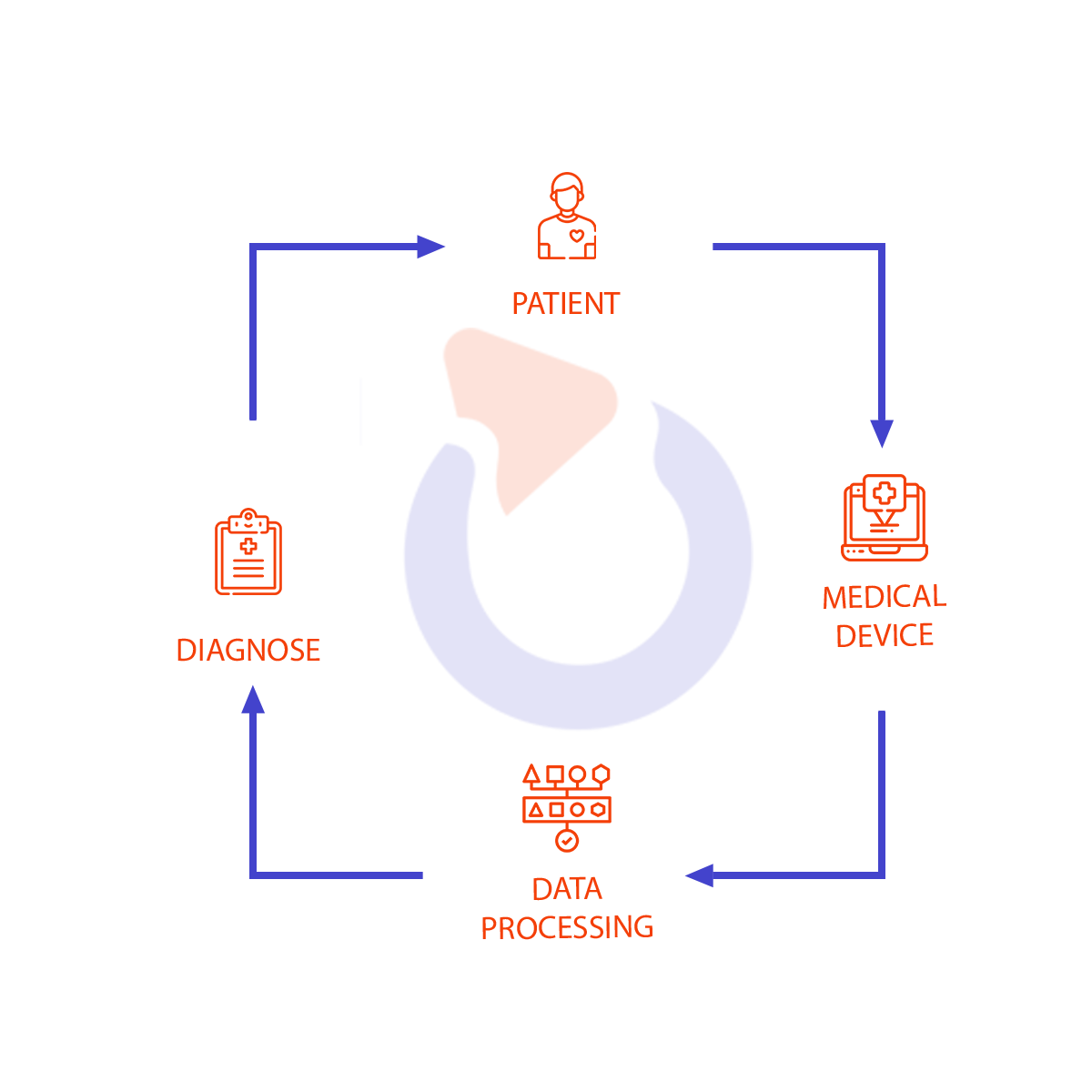
We build complete, end-to-end, solutions starting from the design of the device, its hardware and software development up to the end-user interfaces. We connect to network wearable devices and in vivo transmitters to reduce the need for direct contact between a doctor and patient. This is especially important in the pandemic.
As you can see, most of the process doesn’t require any output from the patient which means that they can simply focus on getting better and not worry about sending their results to different medical facilities or booking multiple visits to get their diagnosis.
This is also better for medical professionals. All patient data is stored in one place and can be accessed at any time. This way, the doctor can spend more time supporting the patient, explaining their results and setting up treatment that would meet their needs and any external conditions.
It’s traditional medicine, not telemedicine, that will prepare us for the next outbreak
This is potentially the most important benefit of using telemedicine. As is the case with most coronaviruses, Covid-19 is also likely to come back in waves. It means that the better we prepare ourselves and the better our telemedicine solutions become right now, the easier it will be to treat patients in the future.
We need to push for developing the telehealth sector, all the while making sure that traditional medical facilities such as hospitals are well-prepared and equipped with the newest technology to take care of the most severe cases.
The lifecycle for most telemedicine products tends to be much shorter than that of traditional medical solutions. This means that current conditions with the pandemic forcing companies to quickly come up with new digital products and features. At Spyrosoft, we’re using a process called rapid prototyping where we spend 4 – 8 weeks on researching, prototyping and validating ideas to finally bring them to life and test them out with real patients.
Telemedicine doesn’t address the limited access to tests
While telemedicine is great for conditions that don’t need complex procedures, what if a patient needs a test?
One answer to this problem is using at-home testing kits widely. That of course means making the kits easy to use and simplifying the procedure. And it’s what happens to any type of test, ranging from genetic dispositions to vitamin and minerals deficiencies. However, the technology is still not perfect, and some experts say that at-home testing kits still need more accessible user information provided with them and better smart return delivery methods. They have not yet reduced the burden put on hospitals and testing labs, but they allow people to take necessary precautions and check their health without needing to queue up at physical locations.
Another way to tackle the issue of limited access to testing is by combining traditional medicine with telehealth. This hybrid method would involve setting up mobile testing labs that can be placed at schools and/or public offices or in vehicles that could travel to remote locations taking samples and delivering them to medical labs afterward, with the test results being sent to a patient via a text message or email.
Telemedicine doesn’t address the lack of medical equipment
The lack of telemedicine equipment is stopping the industry from growing. As is the case with at-home tests, medical hardware also must become more accessible and easier to use at home or in any type of environment with compromised conditions (unstable internet connection or limited access to electricity).
Wrapping up
With 50% of people worldwide (according to WHO and World Bank survey from 2017) still having limited access to essential health services and the perspective that Covid-19 is here to stay, we now need the telemedicine sector to step up more than ever. It’s also the industry where we’ll see exponential growth in the near future.
If you have any telehealth projects to develop, now is the perfect time to start. Get in touch with Spyrosoft Health and Life Sciences Director, Krzysztof Minicki for more information.
About the author
Contact us